First Responder Research Column – The Importance of Adequate Sleep for First Responders’ Mental Health
by Sarah Lanham, MS, CSCS,*D, and Mark Abel, PhD, CSCS,*D, TSAC-F,*D
TSAC Report
October 2025
Vol 78, Issue 1
This column evaluates a unique investigation that describes and compares sleep and associated mental health outcomes across first responder occupations.
Overview
Behavioral and mental health concerns are prevalent among first responders, with a suicidal ideation rate nearly 10 times greater than the United States’ general population (1,6). Identifying modifiable factors associated with mental health outcomes, like sleep, is critical to support first responders. Unfortunately, occupational factors are associated with reduced sleep quantity and quality among first responders (7,18). This column evaluates a unique investigation that describes and compares sleep and associated mental health outcomes across first responder occupations. The findings inform the need for sleep interventions among first responders.
SLEEP QUALITY AND MENTAL DISORDER SYMPTOMS AMONG CANADIAN PUBLIC SAFETY PERSONNEL. INTERNATIONAL JOURNAL OF ENVIRONMENTAL RESEARCH AND PUBLIC HEALTH 17(8): 2708, 2020.
ANGEHRN, A, TEALE SAPACH, MJN, RICCIARDELLI, R, MACPHEE, RS, ANDERSON, GS, AND CARLETON, RN
BOTTOM LINE UP FRONT (BLUF)
On average, public safety personnel (PSP) did not obtain adequate amounts of sleep for health benefits during work nights and nearly 50% of PSPs screened positive for a mental health disorder. In addition, poor sleep quality was associated with numerous mental health disorders, alcohol use disorder, and occupational stress.
Behavioral health concerns and mental health disorders are prevalent among first responders (1,6). Insufficient sleep is associated with comorbidities including mental health disorders in the general population, with a third of US adults reporting insufficient sleep duration (less than seven hours) (11,15). More critically, 27% of United States adults suffer from insomnia, which is associated with 9 – 17 times greater risk of clinical depression, anxiety, and significant decrements in quality of life (10,15). However, there is limited research describing sleep outcomes between first responder personnel types and evaluating the relationship of sleep outcomes with mental health disorders. Therefore, the purpose of this study was to evaluate sleep and mental health outcomes across first responder personnel.
In the final analysis, 5,813 (66% men, 34% women) PSPs completed sleep items as part of an online survey that comprised the data set for this study. PSPs were categorized as municipal/provincial police (26%), Royal Canadian Mounted Police (RCMP; 26%), correctional workers (14%), firefighters (career and volunteer; 15%), paramedics (14%), and communications officials (5%). Regarding demographics, the largest distribution of responders were 39 – 49 years of age (37%), married (75%), white ethnicity (91%), and had some post-secondary education (54%).
The following measures were used to describe sleep and mental health outcomes. The Insomnia Severity Index was utilized as a measure of sleep quality by using seven items that rate the level of satisfaction with “your current sleep pattern” (0 = “very satisfied” to 4 = “very dissatisfied”) (3). A score of 10 or more indicates clinically significant distress (3). The Posttraumatic Stress Disorder (PTSD) Checklist for Diagnostic and Statistical Manual of Mental Disorders 5 was used to assess PTSD symptoms experienced over the last month (0 = “not at all” to 4 = “extremely”) (17). The Patient Health Questionnaire utilizes nine items (0 = “not at all” to 3 = “nearly every day”) to assess the frequency of depressive symptoms experienced over the past two weeks (8). The General Anxiety Disorder Scale was used to evaluate symptoms of anxiety (0 = “not at all” to 3 = “nearly every day”) (14). The Alcohol Use Disorders Identification Test was utilized and scored items based on alcohol consumption frequency (12). Social anxiety was evaluated with the Social Interaction Phobia Scale (4). Panic disorder symptoms were assessed using the Panic Disorder Severity Scale (13). Finally, shift work stress was evaluated with a single item—“Please indicate how much stress shift work has caused you over the past 6 months” (0 = “no stress” to 6 = “a lot of stress”).
Over half of all tested PSPs (56%) screened positive for insomnia. Firefighters screened positive for insomnia the least, although still nearly half (49%), whereas paramedics screened positive the most (60%). On average, all of the PSPs except firefighters exceeded the minimal threshold on the Insomnia Severity Index, indicating clinically significant distress. On average, the PSP sample obtained less sleep during work nights (6.2 hr) than off-shift nights (7.2 hr). Across PSP categories, the average amount of sleep during work nights (range across all PSP category averages: 6.0 – 6.3 hr), off-shift nights (7.0 – 7.6 hr), days feeling rested (2.1 – 2.7 d), and quality of sleep rating (2.8 – 2.9) was remarkably similar. About half of all PSPs screened positive for at least one mental health disorder, ranging from 44% (communications officials) to 56% (correctional workers). Interestingly, firefighters tended to report lower levels of PTSD, depression, anxiety, social anxiety disorder, panic disorder, and a higher level of alcohol use disorder compared to other PSPs. Whereas, on average, RCMP and correctional workers tended to report higher levels of PTSD, depression, anxiety, social anxiety disorder, panic disorder, and a lower level of alcohol use disorder. There is no indication of a statistical comparison across groups, thus it is not possible to determine if these are significant differences. Paramedics, communications officials, RCMP, and correctional workers reported significantly more sleep disturbances than firefighters and municipal/provincial police officers (p<0.01). Among all PSPs, screening positive for insomnia increased the likelihood of screening positive for a mental disorder by 3.4 – 7.0 times (p<0.001). Sleep quality was also related to PTSD, depression, anxiety, social anxiety disorder, panic disorder, and alcohol use disorder (p<0.01). Finally, occupational stress was associated with sleep duration and quality (p<0.01).
RELEVANCE FOR THE TACTICAL FACILITATOR
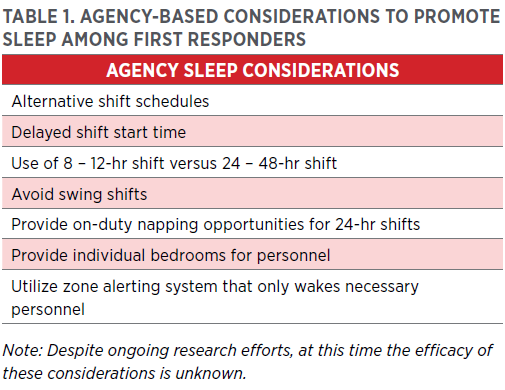
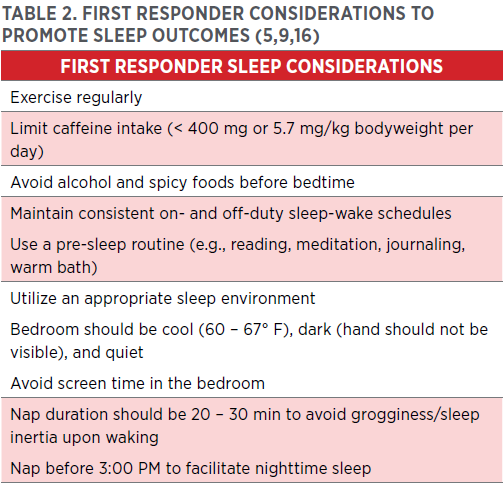
The findings from this study indicate that, regardless of occupational type, first responders do not obtain adequate amounts of sleep for physical health and that sleep outcomes are associated with mental health disorders and perceived occupational stress. Although informative, it is important to note that these cross-sectional relationships do not infer causality. Regardless, tactical facilitators and first responder agencies should consider utilizing a comprehensive approach to promote positive departmental wellness culture while reducing barriers to preventative (e.g., educational resources and support groups) and early intervention mental healthcare (e.g., screening and access to specialists), which play a critical role in addressing mental health outcomes (2). However, relevant to this investigation, agency stakeholders should consider implementing appropriate sleep-based countermeasures. Table 1 provides examples for agency-based considerations. In addition, proper sleep hygiene is important to enhance sleep outcomes. Table 2 provides a list of suggestions to enhance sleep outcomes for first responders (9,16). In summary, sleep is critical for all first responders and agencies should facilitate and promote healthy sleep practices.
This article originally appeared in TSAC Report, the NSCA’s quarterly, online-only publication geared toward the training of tactical athletes, operators, and facilitators. It provides research-based articles, performance drills, and conditioning techniques for operational, tactical athletes. The TSAC Report is only available for NSCA Members. Read more articles from TSAC Report
References
- Abbot, C, Barber, E, Burke, B, Harvey, J, Newland, C, Rose, M, and Young, A. What’s killing our medics? Ambulance Service Manager Program. Conifer, CO: Reviving responders. 2015. Retrieved March 2025 from https://www.revivingresponders.com/originalpaper.
- Barger, LK, O’Brien, CS, Rajaratnam, SMW, Qadri, S, Sullivan, JP, Wang, W, et al. Implementing a sleep health education and sleep disorders screening program in fire departments: A comparison of methodology. Journal of Occupational and Environmental Medicine 58(6): 601-609, 2016.
- Bastien, CH, Vallières, A, and Morin, CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine 2: 297-307, 2001.
- Carleton, RN, Collimore, KC, Asmundson, GJ, McCabe, RE, Rowa, K, and Antony, MM. Refining and validating the social interaction anxiety scale and the social phobia scale. Depression and Anxiety 26(2): E71-E81, 2009.
- European Food Safety Authority. EFSA scientific opinion on the safety of caffeine. 2015. Retrieved June 2025 from https://www.efsa.europa.eu/sites/default/files/corporate_publications/files/efsaexplainscaffeine150527.pdf.
- Jetelina, KK, Molsberry, RJ, Gonzalez, JR, Beauchamp, AM, and Hall, T. Prevalence of mental illness and mental health care use among police officers. Journal of the American Medical Association Network Open 3(10): e2019658, 2020.
- Jones, S. Describing the mental health profile of first responders: A systematic review. Journal of the American Psychiatric Nurses Association23(3): 200-214, 2017.
- Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: Validity of a brief depression severity measure. International Journal of General Medicine 16(9): 606-613, 2001.
- Mayo Clinic. Napping: Do’s and don’ts for healthy adults. Retrieved March 2025 from https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/napping/art-20048319.
- Olfson, M, Wall, M, Liu, SM, Morin, CM, and Blanco, C. Insomnia and impaired quality of life in the United States. The Journal of Clinical Psychiatry79(5): 12020, 2018.
- Pankowska, MM, Lu, H, Wheaton, AG, Liu, Y, Lee, B, Greenlund, KJ, and Carlson, SA. Prevalence and geographic patterns of self-reported short sleep duration among US adults. Preventing Chronic Disease 20: e53, 2023.
- Saunders, JB, Aasland, OG, Babor, TF, de la Fuente, JR, and Grant, M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addiction 88(6): 791-804, 1993.
- Shear, MK, Brown, TA, Barlow, DH, Money, R, Sholomskas, DE, Woods, SW, et al. Multicenter collaborative panic disorder severity scale. American Journal of Psychiatry 154(11): 1571-1575, 1997.
- Spitzer, RL, Kroenke, K, Williams, JB, and Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine 166(10): 1092-1097, 2006.
- Taylor, DJ, Lichstein, KL, Durrence, HH, Reidel, BW, and Bush, AJ. Epidemiology of insomnia, depression, and anxiety. Sleep 28(11): 1457-1464, 2005.
- The National Sleep Foundation. How much sleep do you really need? 2020. Retrieved March 2025 from https://www.thensf.org/how-many-hours-of-sleep-do-you-really-need/.
- Weathers, FW, Litz, BT, Keane, T, Palmieri, PA, Marx, BP, and Schnurr, PP. The PTSD checklist for DSM-5 (PCL-5), 2013. Retrieved March 2025 from https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp#obtain.
- Yoo, H, and Franke, WD. Sleep habits, mental health, and the metabolic syndrome in law enforcement officers. Journal of Occupational and Environmental Medicine 55(1): 99-103, 2013.
Learn about the benefits of NSCA Membership »
TSAC Facilitators
Exercise Science Program design Organization and Administration Testing and Evaluation Client Consultation|Assessment Safety Basic Pathophysiology and Science of Health Status or Condition and Disorder or Disease Professional Development
Public Safety Sleep Intervention Depression Sleep Disorders Insomnia Occupational stress Mental Health First Responder
- Privacy Policy
- Your Privacy Choices
- Terms of Use
- Retraction and Correction Policy
- © 2026 National Strength and Conditioning Association